In 1632, some 700 Puritan colonists made the long journey from England to Massachusetts. Their leaders were University of Cambridge alumni looking for opportunities in a far-away land – and they called their new settlement “Cambridge” after the ancient University. John Lambert’s career has taken a similar (though less perilous) path – beginning at Christ’s College Cambridge in the UK in 1969 and still going strong in Cambridge, Massachusetts, on the banks of the Charles River. And though Lambert says he can’t claim a history quite as exciting as those original colonists who sailed out for the New World (but he’s probably spent more time on the water given his love of rowing!), he has been able to watch – and help – the antibody-drug conjugate (ADC) field develop from a concept into real therapies. Here, Lambert shares his lessons learned.

It’s good to expand your horizons
My studies at Cambridge consolidated my love for biochemistry and also kindled my second passion – rowing (see box: A second love). After completing my PhD in 1976, I made my first voyage to the States to work as a post-doc at the University of California, Davis, where I worked on ribosome structure – specifically the use of cross-linking agents to map ribosomal proteins. After that, I returned to the UK to do a second post-doc at the University of Glasgow, from 1980 to 1982, working on a multi-enzyme complex. Although I wasn’t aware at the time, I was laying the foundations for a career in ADC development. I actually wanted to stay in the UK as a lecturer in biochemistry, but university grants were being cut at that time, forcing me to consider alternatives. The US biotech industry was booming in the early 80s and seemed like a good opportunity. I ended up responding to an advertisement in the journal Science in 1981 for a position at the Sidney Farber Cancer Institute (now Dana Farber Cancer Institute) for a project that aimed to exploit the specificity of monoclonal antibodies – which had only just been invented – to deliver toxic agents to cancer cells. As a protein chemist, I was familiar with conjugation and I had modified proteins and antibodies to analyze their structure, function and activity. So my experience fit the idea of applying the concept of antibody-drug conjugates to the goal of making medicines. I got the job and have stayed in the US – and the field – ever since!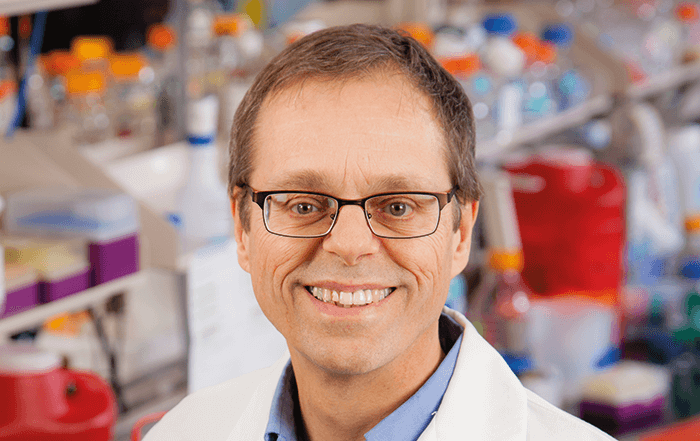
Persevere!
Although I was technically an employee of the Sidney Farber Cancer Institute (SFCI) when I arrived to begin my job in March 1982, I had, for all intents and purposes, joined ImmunoGen, a company specializing in ADCs, as its second scientist, joining Swiss chemist Dr Walter Blattler to build up the research team. At the SFCI, we were answerable to ImmunoGen’s scientific advisory board and the company’s investors paid a grant to SFCI that covered our costs – including wages, materials and equipment. This is essentially how the company started. Then in 1987, a second round of financing came in and we moved into ImmunoGen’s own labs in Cambridge, Massachusetts, and became employees of ImmunoGen directly. We were early movers in the ADC field. The 1980s was the era of mouse monoclonal antibodies and humanization hadn’t yet been invented. Our initial idea was to use mouse antibodies conjugated to derivatives of potent protein toxins – ricin in particular. Unfortunately, we found those to be highly immunogenic in the clinic and realized that we needed to invent a method for humanization. In collaboration with Professor Anthony Rees, who was at the time head of the department of biochemistry at the University of Bath, UK, we developed a humanization method called “resurfacing.” It essentially allowed us to make antibodies non-immunogenic in humans – the first of two major hurdles in developing an effective ADC. The second hurdle was choosing the right agent to link to the antibody. The chemotherapeutic agents at that time were not potent enough to kill cancer cells when attached to antibodies, when one calculates the number of antibody molecules that can be bound by tumor cells following biodistribution of the antibodies in the body. Thinking back to our original plan of using potent toxins like ricin – where attaching one molecule of ricin per antibody certainly made a potent antibody-payload conjugate – we explored whether we could identify small molecular weight compounds that were as potent as ricin, and adapt them for conjugation to our humanized antibodies. The combination would allow us to target cancer cells with a potent toxin without eliciting a host immune response, while minimizing exposure of other tissues to potent cytotoxic agents. We eventually landed on maytansine – a potent tubulin-binding compound that disrupts microtubule/tubulin dynamics – as a parent drug. The challenge for our chemistry group was to create a maytansine derivative that was linkable to antibodies without destroying the activity of the toxin.Some careers take twists and turns as people’s interests shift over the years, leading them into different roles and industries. I was lucky to fall in love with a field fairly early on, and I’ve spent the majority of my career working in ADC development. It’s been fascinating to watch as we overcame the technical hurdles – learning how to humanize antibodies and select the right therapeutic agents – culminating in the approval of Kadcyla. Few other things in my life have managed to keep my interest for so many years – except rowing. I took up rowing at the University of Cambridge when I was 18, and aside from a brief hiatus during my post-doc at UC Davis, rowing has been a part of my life for the subsequent 47 years. I’m currently a member of the Board of Directors for the “Head Of The Charles Regatta” – a two-day event in Cambridge, US, which involves over 12,000 rowers and more than 2000 boats. It takes place on the third or fourth weekend in October (always a pretty time of year with New England fall foliage) on the Charles River and attracts around a 250,000 spectators. I’ve raced in 31 consecutive Head Of The Charles Regattas since 1986! I compete in other races throughout the year, and recently have had success with my doubles partner in lightweight sculling events. At the annual US Masters Championship regatta, we’ve won the lightweight “F” (average age 60 – 64) event for double sculls in both 2012 and 2016. Did I go to Boston for the rowing or the science? Honesty, I went for the science, but I couldn’t believe my luck once I had arrived – there isn’t anywhere better for a rower-slash-scientist in the biotech world! The Pull for a Cure Challenge at the Head Of The Charles regatta aims to raise money for the breast cancer research efforts of the American Cancer Society. You can find out more and even donate at http://tmm.txp.to/0517/pull.
Once we developed our maytansinoid technology for ADCs by the mid-1990s, we knew that if antibody-drug conjugate technologies were going to be successful, HER2 would be a good target. It was already established that HER2 was highly overexpressed on a subset of breast cancers (~20 percent) that were particularly aggressive cancers, and it was under active investigation as a tumor-selective target for antibody-based therapies. Genentech were already in clinical trials at that time with the anti-HER2 antibody trastuzumab, so in the late 1990s we approached them to suggest a collaboration – our maytansinoid payload combined with their HER2-targeting antibody. Ultimately, a deal was struck in 2000. ImmunoGen made several maytansinoid/trastuzumab constructs with a variety of different linker-maytansinoid chemistries, and Genentech evaluated all of them in a variety of preclinical studies in order to select the development candidate, which went into phase I clinical trials in 2006. Ultimately, the pivotal phase III trial data were presented at the American Society of Clinical Oncology (ASCO) in 2012, and the FDA granted a product license to Genentech in February, 2013. It was an exciting moment for ImmunoGen! The product, whose generic name is trastuzumab emtansine, is marketed as Kadcyla for treating HER2-positive breast cancer. To date, Kadcyla is the first and only ADC to receive full approval based on a randomized phase III study.
Always focus on your target
Having worked in ADC development for 35 years, my most important piece of advice is to focus on the target – and Kadcyla illustrates this point well. Because we used an already approved antibody – trastuzumab, marketed as Herceptin – the development was relatively rapid. Commercial manufacturing of the antibody was already in place. And with a ready-made test to select patients overexpressing the HER2 target protein, patient selection wasn’t something Genentech really had to think about in early clinical development. Selecting the right patients who could potentially benefit from treatment was important for its rapid clinical development. A couple of ADCs have received accelerated approval after phase II studies for treating hematologic malignancies. Pfizer’s gemtuzumab ozogamicin (Mylotarg) is one, but its approval for treating acute myeloid leukemia in 2000 was withdrawn in 2010 after an unsuccessful confirmatory phase III study (although recently, Pfizer has re-submitted a marketing application to FDA on the basis of subsequent phase III studies that have shown clinical benefit). The second ADC to be approved was brentuximab vedotin (Adcetris) marketed by Seattle Genetics and Takeda for treating Hodgkin lymphoma and systemic anaplastic large cell lymphoma. Hematologic malignancies generally have well-defined lineage-specific targets. The emerging data for solid tumors seem to support the hypothesis that greater antigen density increases the effectiveness of the ADC. Higher target expression leads to more ADC accumulation at the tumor, and more uptake of ADC into cells on a per cell basis. So one of the key lessons we’ve learned was that target expression is very important when thinking about the application of ADC technology to cancer patients. In retrospect, if some of those early, discontinued, ADCs had applied better patient selection in early clinical trials, they may have been viable agents.