The deeper we explore human physiology, the more complexity we uncover. To overcome diseases, such as cancer, our approaches have also become more complex, moving far beyond small molecules, chemotherapies, and radiation into protein-based therapeutics.
The infinite variation allowed by peptide architectures almost always ensures that there is a protein-based therapeutic approach for any disease we choose to address. For example, immune checkpoint modulators orchestrate and help restore cell-mediated immune responses, while immunoconjugates help traffic radioisotopes or toxins to specific tumor cell receptors; monoclonal antibodies bind and inhibit TNF-α to treat various autoimmune diseases or IL-2 on activated T cells to prevent kidney transplant rejection.

Beyond these examples are cytokine therapies, fusion proteins, peptide hormones, hemolytic factors, and many more. The variations, applications and complexity of protein-based therapeutics are virtually endless. But they come at a price: complex protein-based therapeutics are difficult to develop. Since the first FDA approval of a mAb (muromonab-CD3) in 1986, there have only been around 350 approved protein-based therapeutics out of a total of nearly 4,500 FDA approved drugs, and only a dozen or so bispecific antibodies, which are a little more complex than the conventional mAbs.
That situation is beginning to change thanks to the advent of mRNA-encoded protein therapeutics. An mRNA-based approach – delivering mRNA molecules that have been engineered to express a therapeutic protein in vivo — overcomes many of the limitations and challenges associated with the traditional recombinant approach to protein design and delivery.
mRNA-encoded protein therapeutics also offer further advantages beyond design, in terms of dosing, manufacturing quality, native post translational modifications (for example, glycosylation), and therapeutic applicability across a variety of indications and tissues. In this article, we provide an overview of the challenges associated with traditional protein-based therapeutic development, and look at how mRNA-based development overcomes many of those challenges and improves upon the design and delivery of these extraordinary biologics.
Protein-based problems
The traditional method of protein-based therapeutic development is based on recombinant protein expression systems, which have several basic – but significant – limitations. Recombinant proteins require additional time and resources for development of expression cell lines for biomanufacturing. Furthermore, recombinant proteins are fragile species; maintaining protein stability without impinging on drug efficacy throughout development, manufacturing, storage, and delivery to healthcare centers and patients is both labor and resource intensive.
Drug formulations must be developed and tailored to the protein, as well as to individual patient populations, delivery methods, and (in some cases) to differing disease indications. All these factors add to the development timeline – on average 18 months or more for full molecule development, from the transfection of the production cell line to drug product – delaying clinical studies and the eventual delivery of these much-needed therapies to patients. In vivo delivery using an mRNA-based approach eliminates all these manufacturing bottlenecks.
More importantly, while protein-based therapeutics have shown great promise, they remain plagued with several critical physiological challenges. Tumor-specific drug targets are typically overexpressed on cancer cells. However, in many cases, healthy cells also express the tumor targets, albeit at a lower level, complicating the targeting specificity of protein therapies.
Another challenge in designing protein-based therapeutics is the fact that the majority of antigens in cancers are expressed intracellularly. With a recombinant approach to development, proteins necessary to target those antigens – for example high-molecular weight antibodies – are unable to cross the cell membrane. As such, intracellularly expressed antigens are still a largely untapped source of therapeutic targets.
It is well known that differential tumor cell antigen expression and tumor heterogeneity often result in poor therapeutic response in patients. Engineering multi-target, antigen-binding capabilities within a single protein is necessary to overcome this challenge. However, multi-target design is difficult to accomplish with a recombinant approach, creating complex challenges for biomanufacturing, purification, and retaining drug stability.
mRNA-based advantages
CD47, a cell surface protein expressed on multiple cell types, including overexpression in cancer cells, offers an excellent case study in the advantages of an mRNA-based approach to the development of protein-based therapeutics. CD47-expressing cancer cells can evade immune clearance and proliferate when they bind the signal regulatory protein alpha (SIRPα) on myeloid cells, creating a “don’t eat me” signal that causes phagocytic immune cells to mistake the cancer cells for “self” and pass them by. Disrupting this interaction has become an important goal and target in cancer immunotherapeutic development.
However, as a target, the CD47-SIRPα interaction is fraught with barriers. CD47 is broadly expressed at low levels on many healthy cell types. For instance, CD47 is well expressed on red blood cells, which can create off-tumor, on-target activity leading to hematological toxicities in patients. This can dramatically reduce the therapeutic window of drugs that target the CD47-SIRPα interaction. Further, the off-tumor and on-target binding of the anti-CD47 drug can act as a sink, reducing the effective therapeutic concentration.
A promising avenue of development to overcome these barriers is a multivalent approach to complex protein design. For example, engineering an octavalent SIRPα-Fc fusion protein increases CD47 binding (apparent) affinity because of increased avidity (i.e., tighter binding as the target density is increased). This multivalent approach enables the protein to differentiate low versus high target expressing cells with dramatically improved specificity. It achieves a high signal (on-target tumor cell binding) to noise (on-target off-tumor effects) ratio, increasing the therapeutic window and driving potent tumor killing without enhancing binding to low target expressing healthy cells (Figure 1).
mRNA-based engineering of complex proteins can also be used to increase target specificity and circumvent tumor heterogeneity by taking a multi-target approach to protein design. For example, in B cell-mediated diseases, Fc effector function can be enhanced through macrophage checkpoint inhibition via SIRPα. However, off-target binding is still a concern because of the wide expression of CD47 across the immune cell population. A multi-target approach using a trispecific protein – for example, targeting aCD19-aCD20-SIRPα – engages CD47 only when other targets, CD19 and CD20, are present, ensuring that only B cells are targeted out of the total immune cell population. Engaging multiple tumor-associated antigens overcome the tumor heterogeneity, hence results in broader tumor coverage, and enhance cellular specificity, thereby increasing the therapeutic window (Figure 2). In this way, SIRPα-CD47 binding is tuned to avoid off-tumor binding to improve safety (Figure 3).
Other advantages
Multi-valent and multi-target approaches to engineering protein-based therapeutics address the physiological challenges well, but, in theory, a recombinant approach could produce constructs able to manufacture the same types of molecules. So why would one feel compelled to take an mRNA-based approach over recombinant design?
There are several reasons. First, because there is no need to develop expression cell lines, manufacturing and purification protocols, or specific drug formulations, development times for mRNA-based therapeutics are greatly reduced, down to six months from eighteen, on average. Multispecific and multivalent proteins have structural, chemical, and binding properties that can make their manufacturing and purification difficult, when working from recombinant constructs. Precision manufacturing involved in mRNA-based therapeutics also allows for elimination of many of the manufacturing, purification, storage, and formulation concerns, and results in a very high quality of product produced through the native in vivo process with endogenous post translational modifications.
In vivo expression of proteins from mRNA delivered with high specificity to the cells also creates a beneficial PK profile, avoiding the initial high Cmax observed with intravenous bolus delivery of recombinantly produced therapeutic proteins. The high Cmax has been clinically linked to safety issues, such as cytokine release syndrome, in T-cell mediated therapies. Since the “manufacture” of the protein is in vivo, this approach also overcomes the challenges associated with membrane-bound and intracellular targets. In vivo expression of membrane-bound proteins uses cellular protein expression processes and produces a stable protein that is properly transported to the target site through the cell’s native cell localization systems. This also allows for in vivo targeting of intracellular antigens, providing access to a large, untapped pool of potential therapeutic targets.
For the moment, consistent delivery of mRNA with high tissue and cellular specificity is the limiting factor for mRNA-based protein therapies, but as the delivery vehicle technologies improve, broader applicability for the mRNA-based therapeutics will emerge very quickly.
The future of cancer and disease treatment is one of increasing complexity. Protein-based therapeutics will be key to realizing the treatments of tomorrow. mRNA-based protein design offers the most flexible path forward for designing drugs that overcome the barriers and challenges associated with durable treatments. It also offers advantages from a business perspective by driving down development times, moving therapies to the clinic at greater speed, and forging a path toward simplifying the emerging complexity in our understanding of human biology.
The author wishes to thank Shruti Lal, Adrienne Sallets, Srinivasa Bandi, Gowrisudha Adusumilli, Ray Low, and the rest of the NTX-471/2 project team members for their contributions to the data shown in this article.
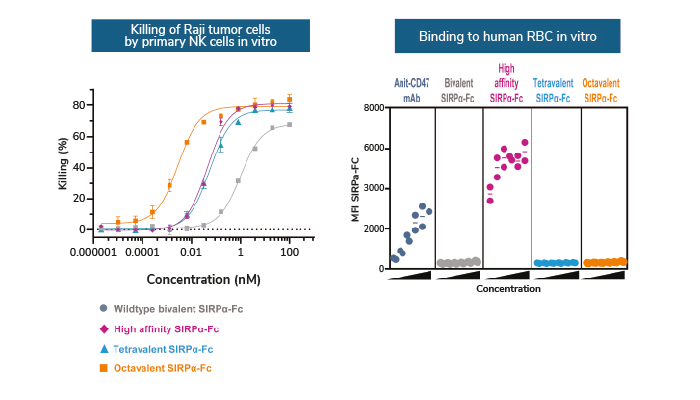
Figure 1. Multivalent SIRPα-Fc molecules enhance potency with minimal impact to healthy cells
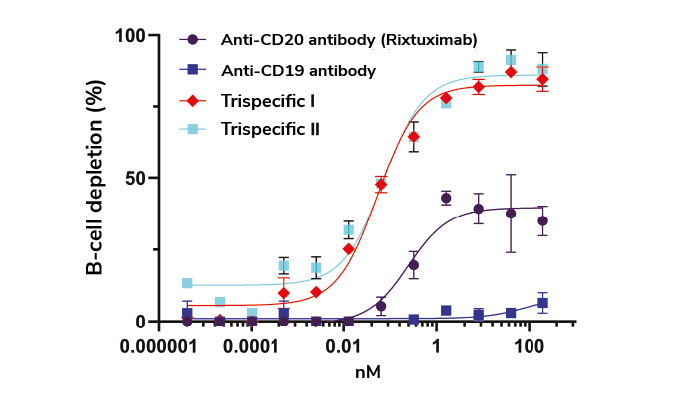
Figure 2. Superior ex vivo B cell depletion in cynomolgus monkey with tri-specific protein designs
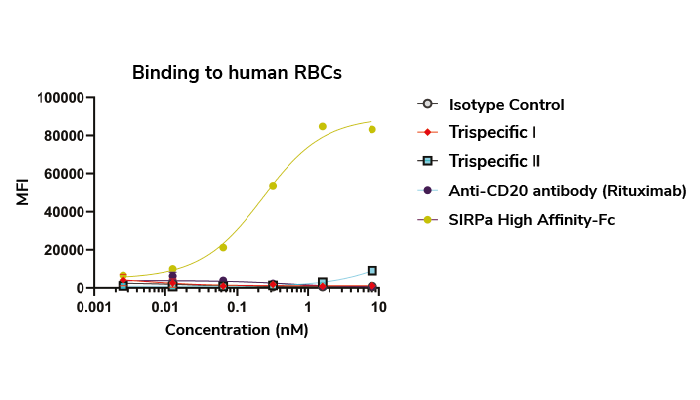
Figure 3. Tri-specific molecules do not bind significantly to human red blood cells